A simple reminder call turned into a front row seat to someone else’s secret life.
Back in 2009, a nursing student worked part time at an orthopedic surgeon’s office. Her tasks stayed boring and routine. She filed charts, called patients, chased down imaging.
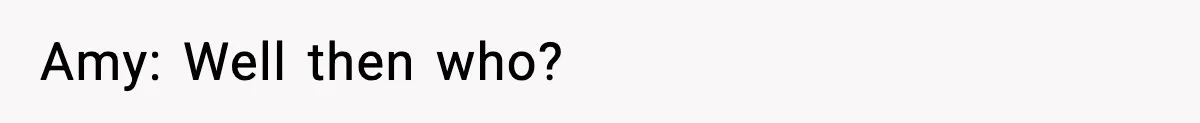
One patient, Frank, needed to bring his MRIs and X-rays for an upcoming surgery. He did not answer. His phone rang and rang.
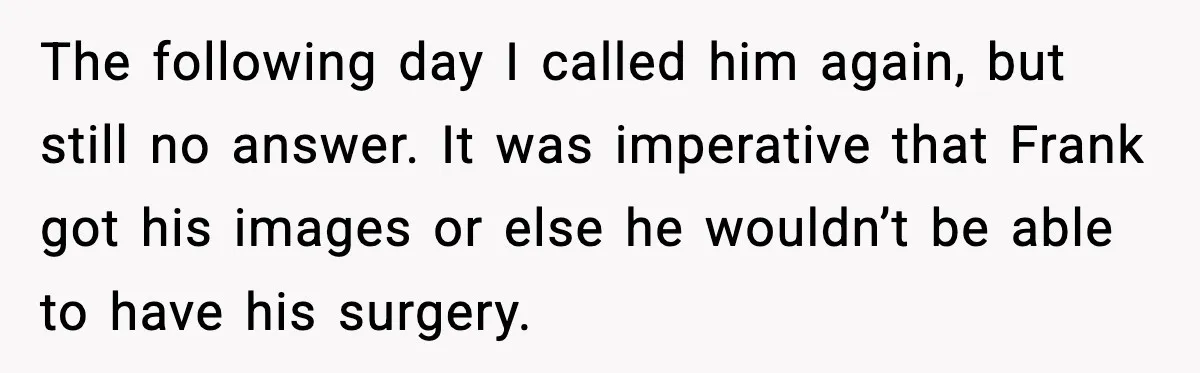
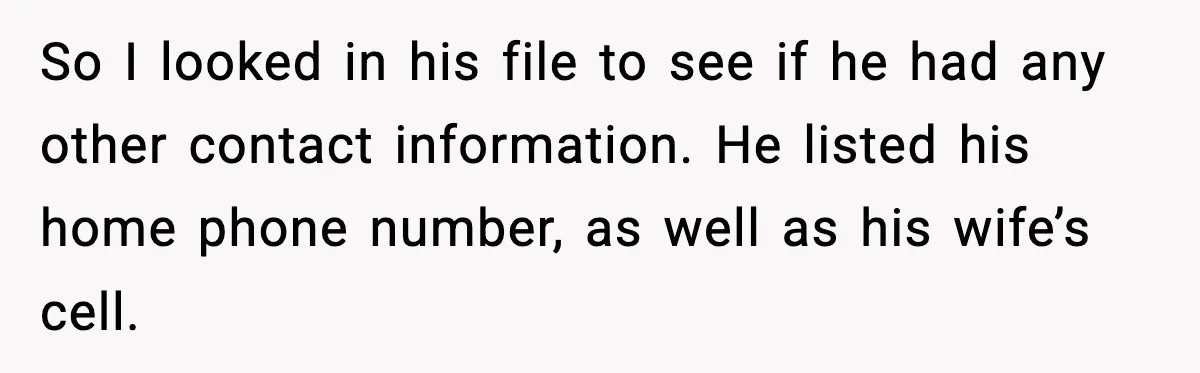
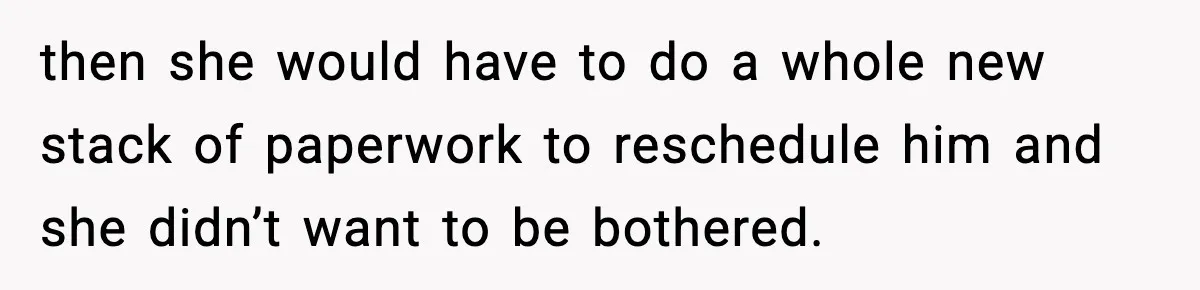
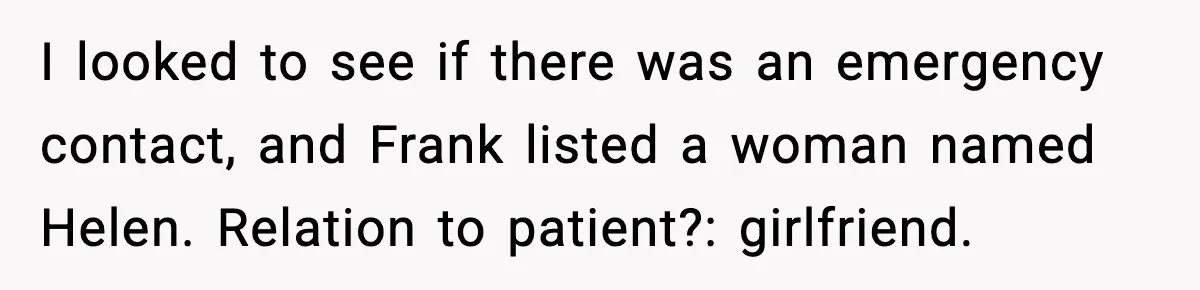
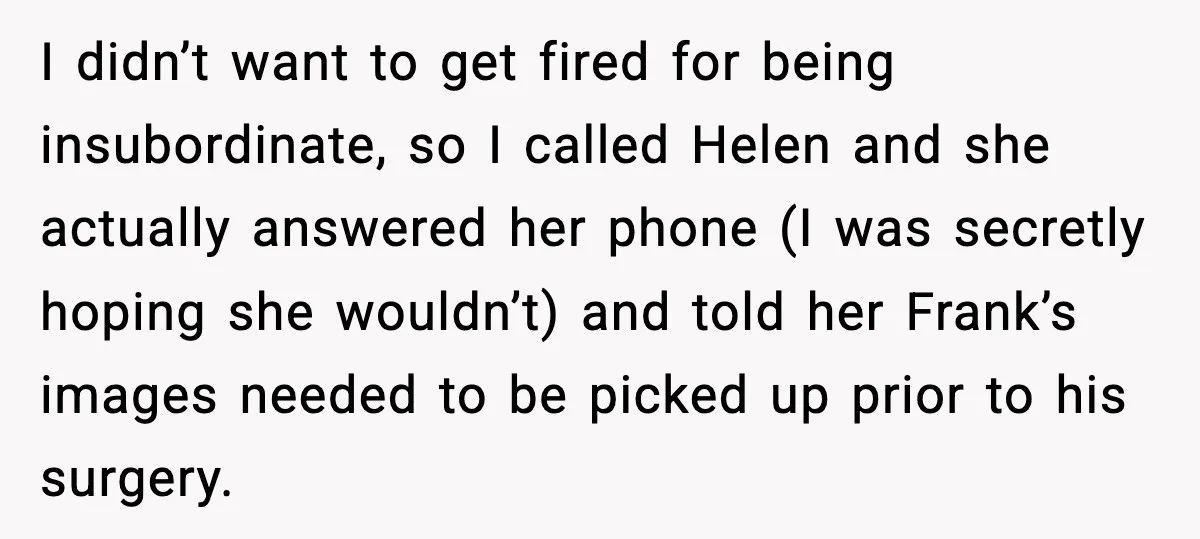
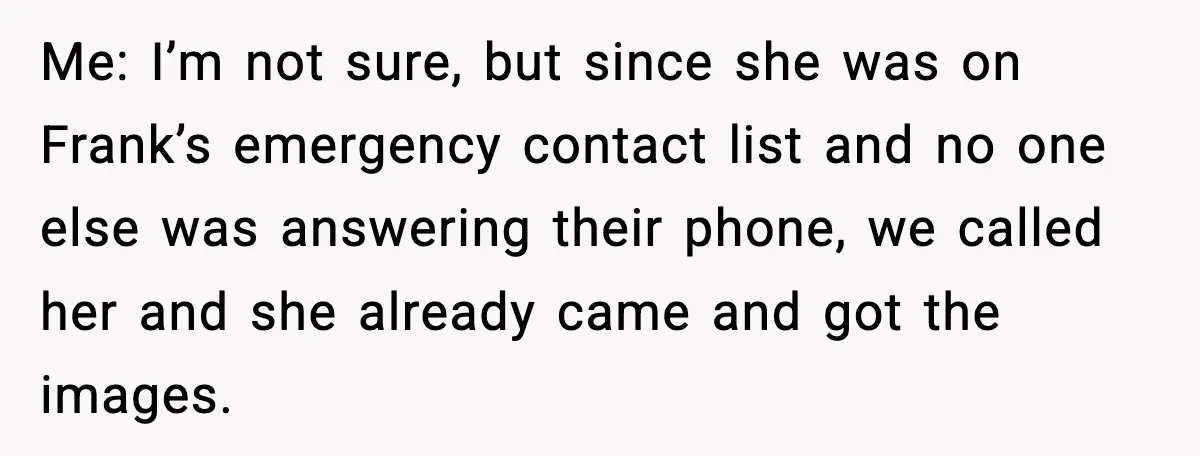
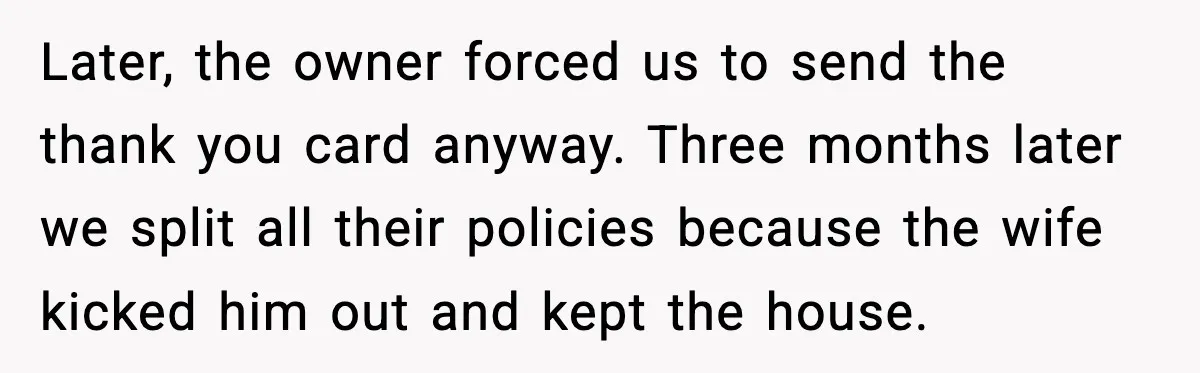
So she did what every medical office does. She checked the chart, called the house, called the wife, followed the manager’s instructions, and then dialed the “emergency contact.”
That contact happened to be a woman labeled “girlfriend.” She picked up, came in, and collected the images. Later, when Frank’s wife called, everything unraveled in real time, right in front of an eighteen year old who only wanted to keep her job and do things right.
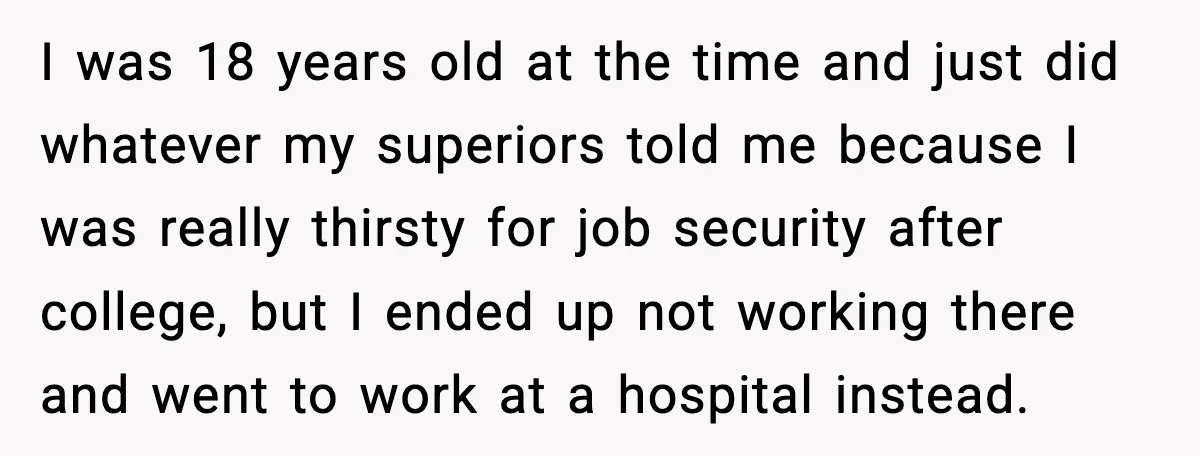
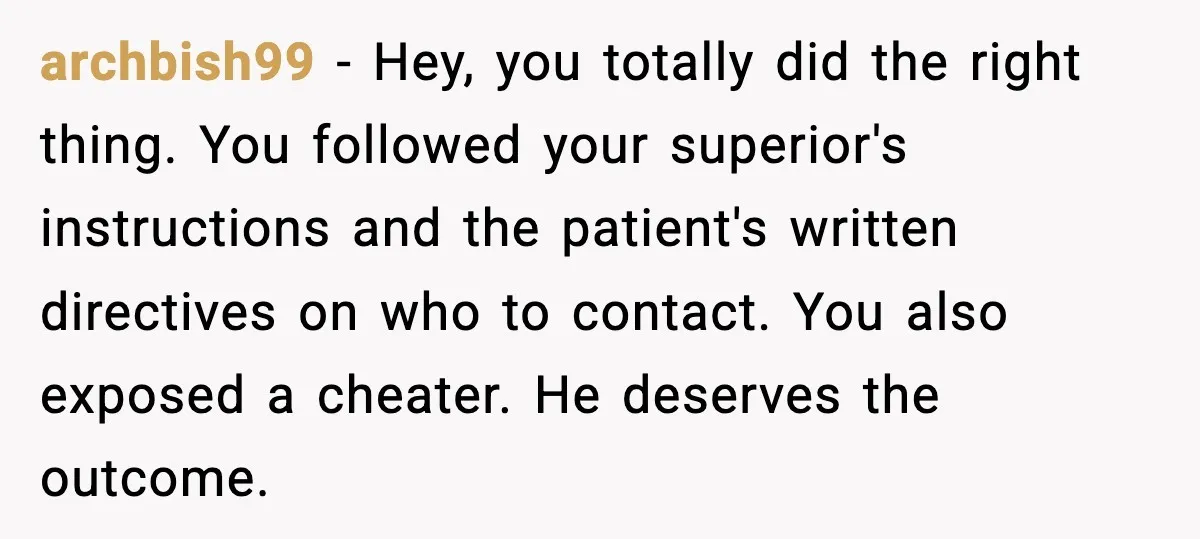
Now, read the full story:


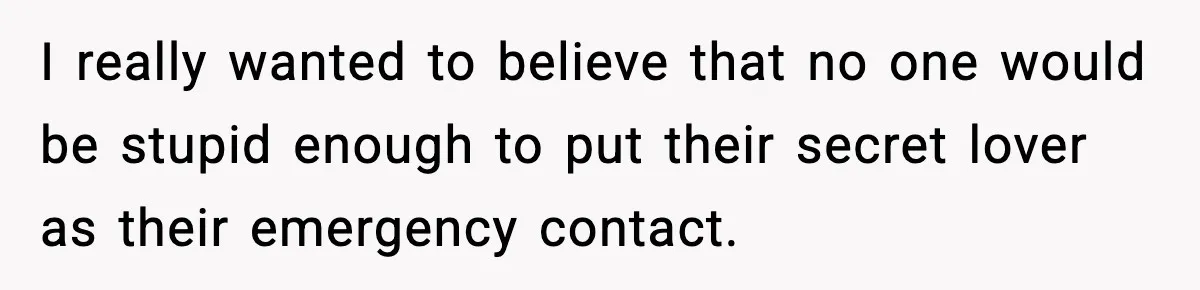
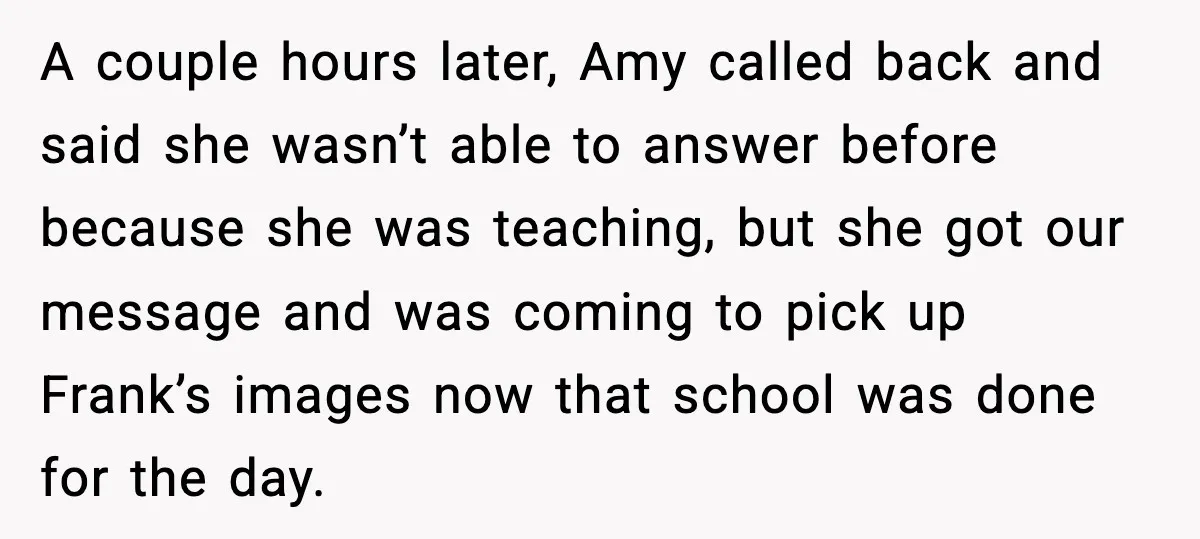
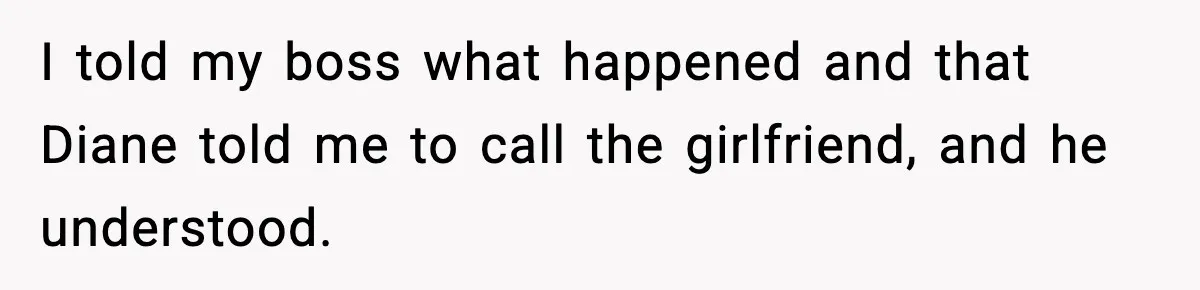
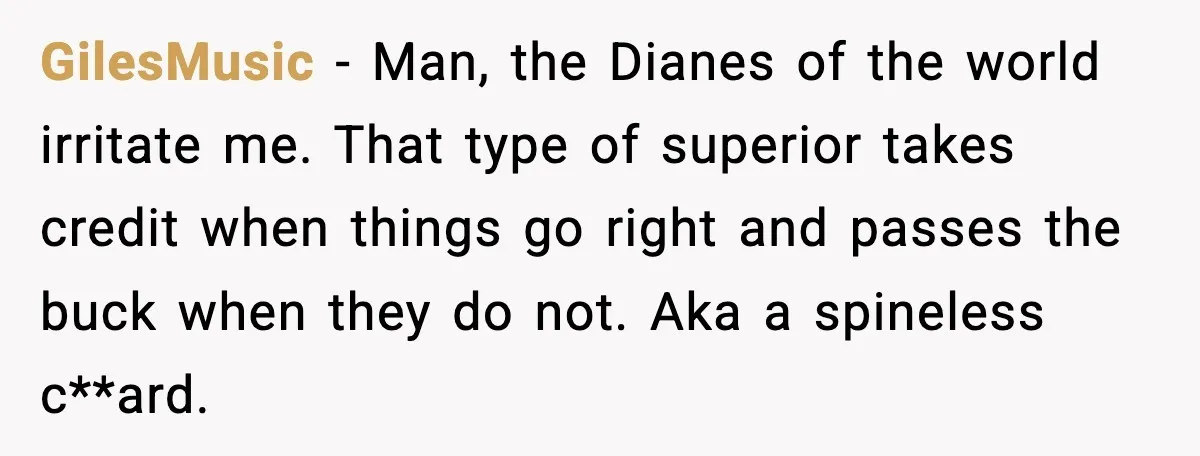
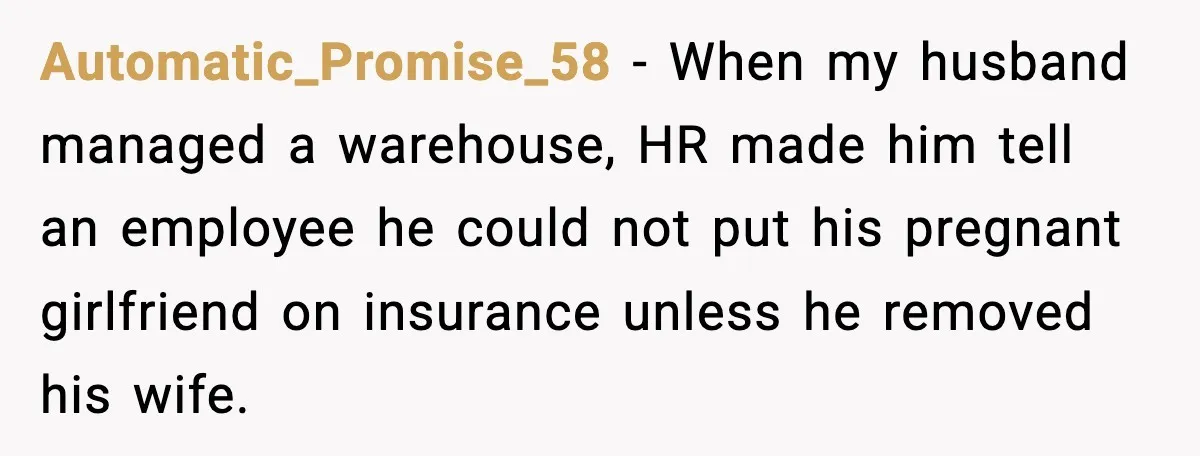
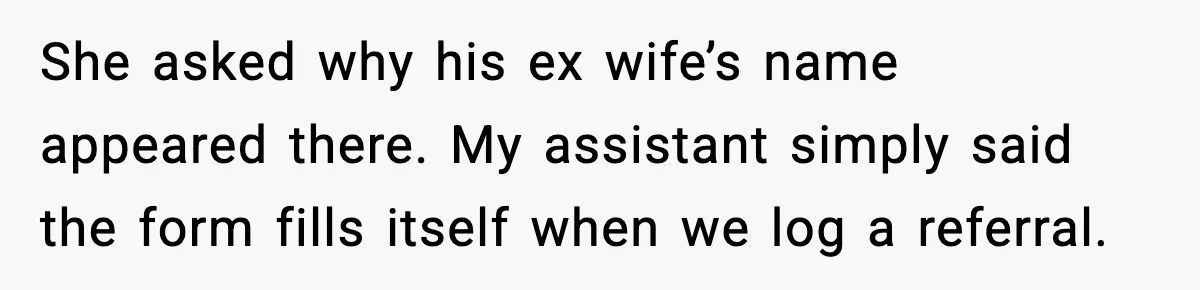
![Cheating Patient Lists Mistress As Emergency Contact And It Backfires Hard Me: [again, trying really hard to be vague] We called someone from his emergency contact list.](https://dailyhighlight.com/wp-content/uploads/2025/11/wp-editor-1763915588304-2.webp)
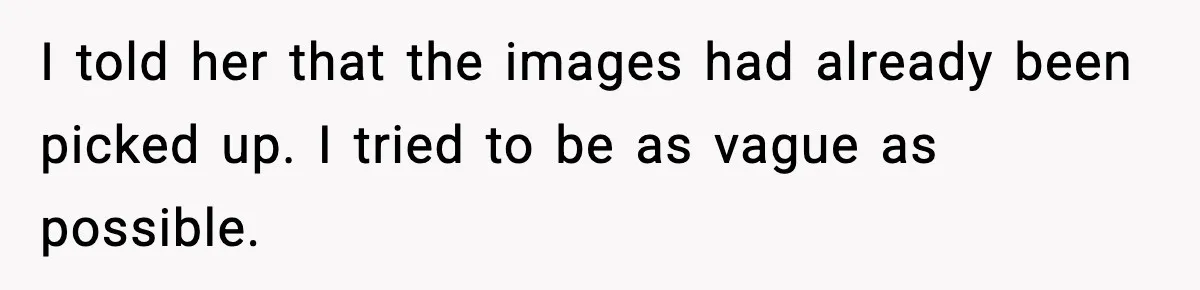
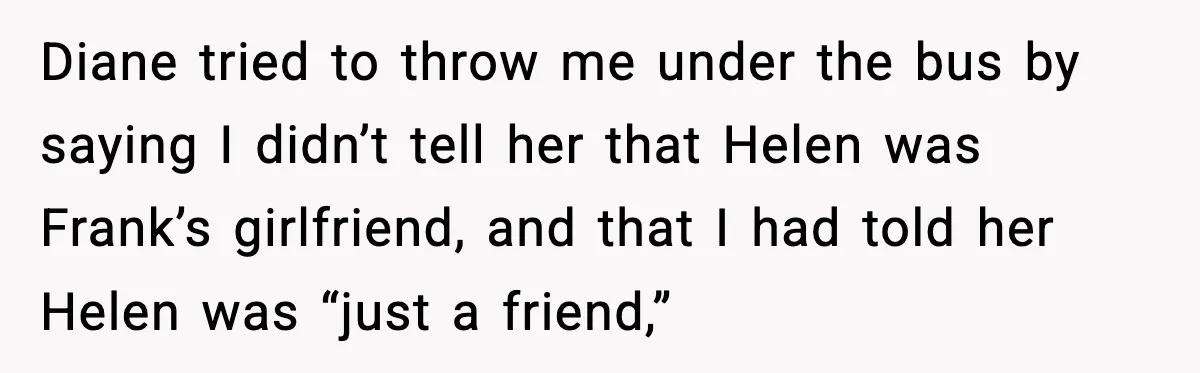
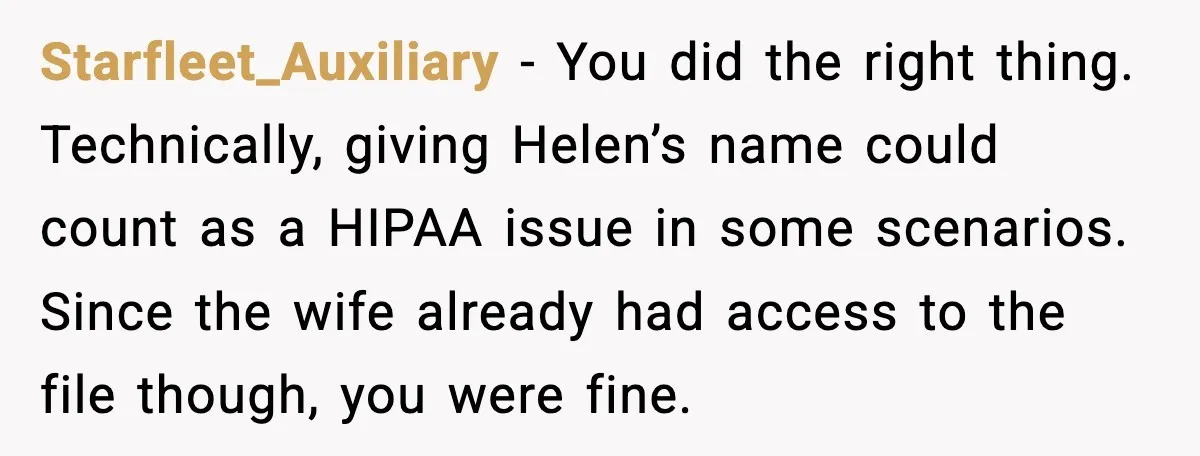
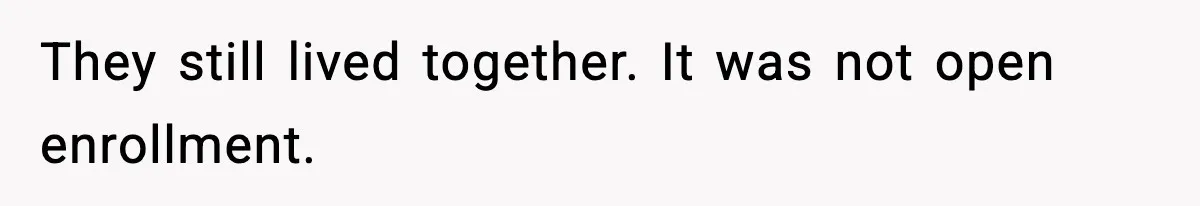
![Cheating Patient Lists Mistress As Emergency Contact And It Backfires Hard Me: [at this point I’m really nervous] No, not his brother.](https://dailyhighlight.com/wp-content/uploads/2025/11/wp-editor-1763915589846-4.webp)


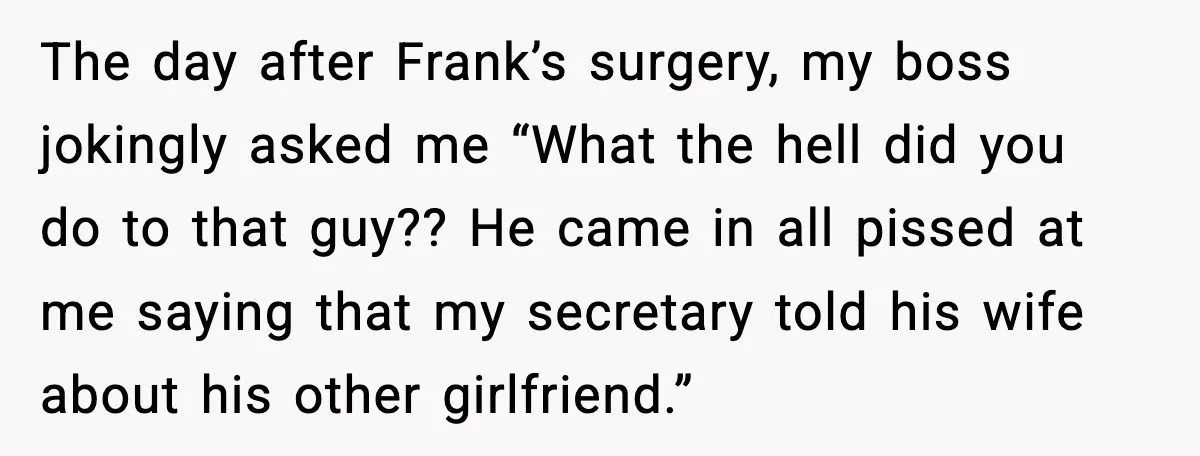
This story hits a very specific nerve for anyone who has worked in healthcare or admin. You can feel OP caught in the middle of three different forces. Her boss’s expectations. Her manager’s orders. Her own sense that this felt messy and wrong.
She tried to protect everyone. She followed policy as it was explained to her. She called the numbers in the chart. She tried to stay vague with the wife. She carried the emotional fallout for a decision that started with Frank’s own choice to list his girlfriend on official paperwork.
There is also a familiar ache in that eighteen year old hunger for job security. Young staff often accept pressure that older workers would push back against. They want to prove themselves, so they absorb the blame and discomfort.
This situation shows moral discomfort more than malice. OP did her job. Frank wrote his own disaster.
Diane tried to dodge responsibility. That mix shows up in workplaces every day, just in quieter ways.
This feeling of being squeezed between “do your job” and “do what feels right” sits at the center of the whole story.
At the heart of this story, three threads twist together. Workplace hierarchy. Patient privacy rules. The emotional fallout of secret relationships.
First, the legal and ethical side. Frank chose Helen as an emergency contact and labeled her “girlfriend.” From a HIPAA perspective, providers may share information with family, friends, or “other persons identified by a patient” when that information directly relates to the person’s involvement in care or payment.
So when the office called an emergency contact listed in the chart about picking up imaging, the staff followed what the law actually allows. The weak point sat in the lack of clear internal policy and training about how much detail to share when multiple partners exist.
The emotional part hits harder. Frank created a land mine by listing his mistress as an emergency contact while still presenting as a married man. Cheating often carries heavy stigma.
Surveys show that around three quarters to almost ninety percent of Americans consider extramarital affairs morally wrong. So when the truth slips out, the reaction tends to explode. That anger often looks for a convenient target.
In this case, he aimed at the doctor’s office instead of his own choices.
For OP, this situation fits the definition of moral distress. Nursing researchers describe moral distress as the feeling you get when you know the ethically sound action, but workplace pressures push you to act differently.
She sensed the awkwardness of calling a listed “girlfriend” when the wife still appeared in the file. She raised the concern to her manager. The manager pushed her to call anyway because paperwork felt more annoying than nuance. That decision placed OP in the line of fire without real power to change the setup.
Studies on moral distress in healthcare show links to frustration, guilt and emotional exhaustion, especially when staff feel stuck between policy and personal values.
Young workers feel this even more sharply because they rely on good references and future opportunities.
They follow orders and hope the people above them will take responsibility if trouble comes.
Psychology also offers a lens here. The classic Milgram obedience experiments showed that many ordinary people obey authority figures, even when the instructions conflict with their own judgment.
OP’s situation looked nothing like a lab shock machine. Yet the dynamic feels similar in miniature. A manager gave a direct instruction. The worker felt uneasy but followed anyway, because she trusted the person in charge and needed the job.
So what does “doing better” look like in real offices?
For clinics and hospitals, the answer starts with training and clear policy. Front desk workers and nurses need simple scripts for messy personal situations.
For example, when multiple partners appear in the record, staff can say, “I am allowed to speak with the person listed here, but I cannot discuss who else is on the file.” If a spouse asks who picked something up, a safer answer is, “An authorized contact already collected it, and everything is in place for the surgery.”
That level of privacy protects staff from becoming accidental messengers of infidelity.
Managers also carry a big share of responsibility. Good leaders listen when junior staff say, “This feels awkward” and help them navigate it instead of dismissing the concern.
A manager like Diane, who pushes a risky choice and then tries to shift blame, damages trust and culture. Research on moral distress in healthcare teams links this kind of leadership to higher turnover and worse collaboration.
For individual workers, some practical steps help. Ask for clarification in writing when a situation feels risky. Use policy language instead of personal opinions on the phone. Request backup from a supervisor when a caller becomes emotional. These habits protect both the patient and the staff member.
The deeper message in this story sits at the intersection of honesty and systems. Frank wanted the convenience of a secret relationship and the safety of a stable marriage. The office wanted efficiency.
The system gave staff just enough power to cause personal fallout, but not enough guidance to avoid it. When people design better systems and leaders respect ethical discomfort, young workers like OP do not have to carry that burden alone.
Check out how the community responded:
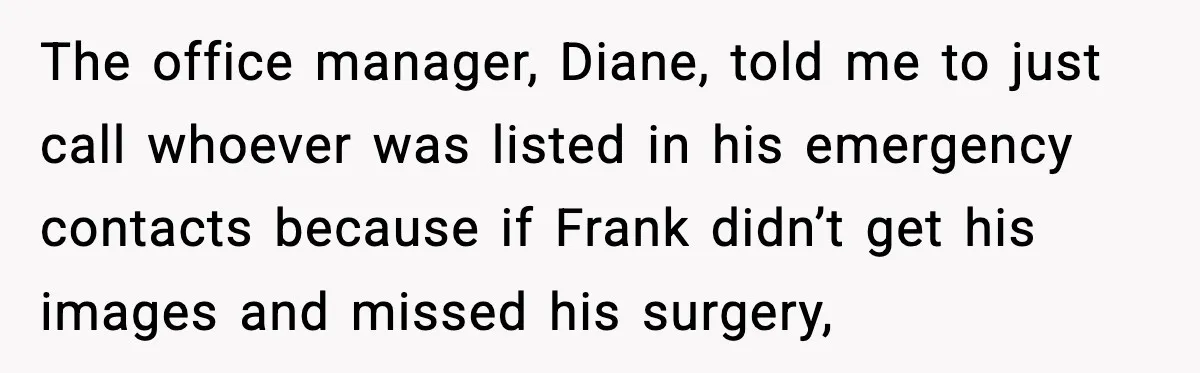
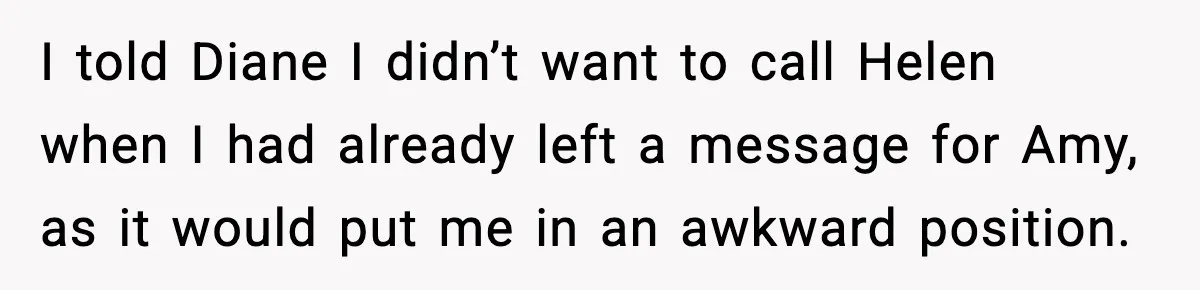
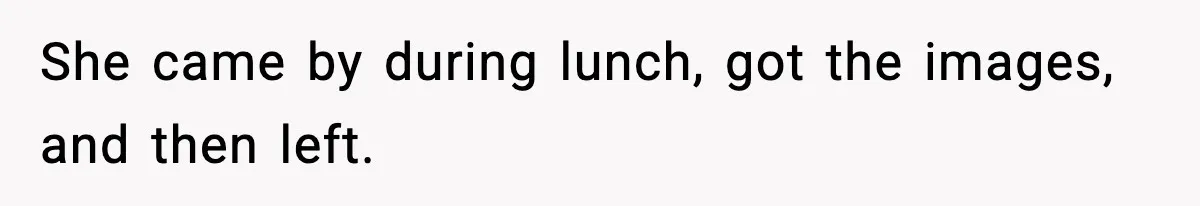
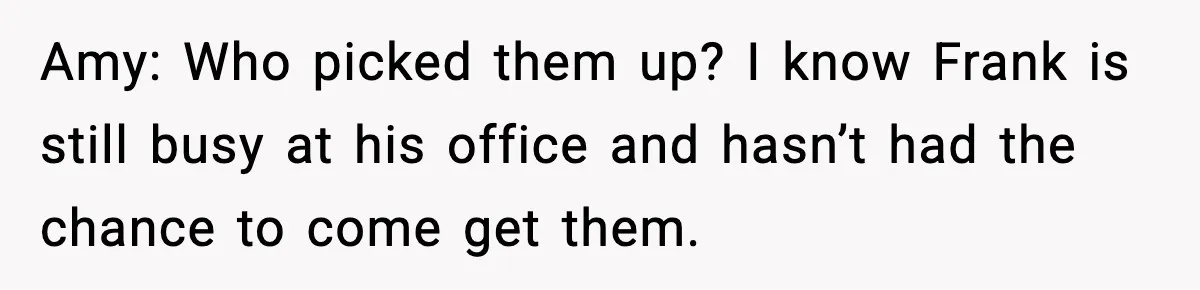
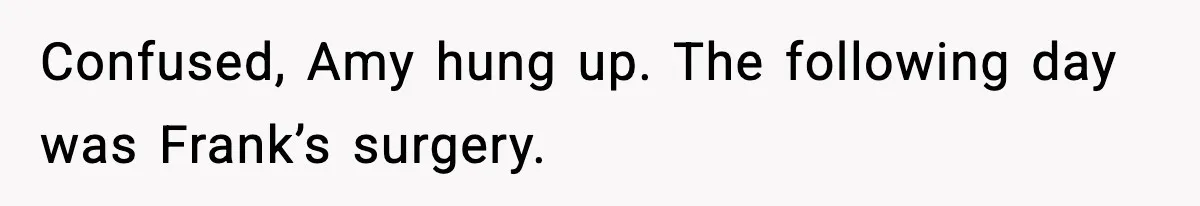
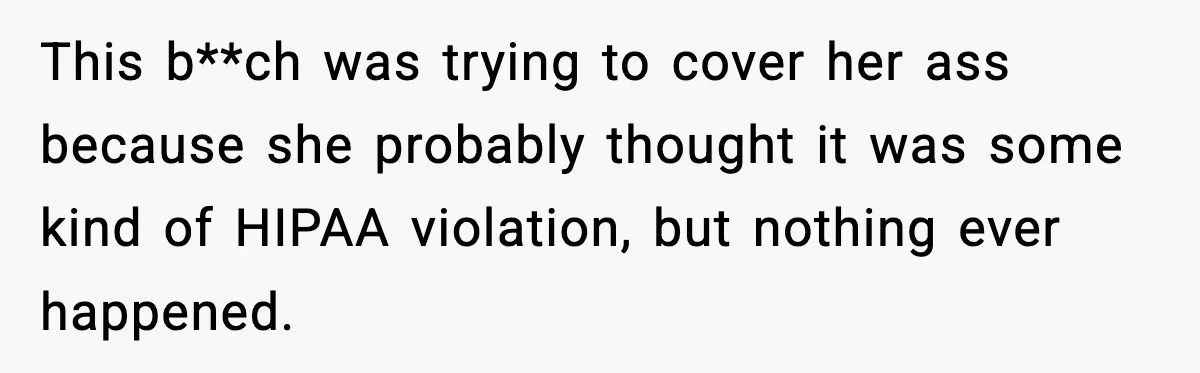
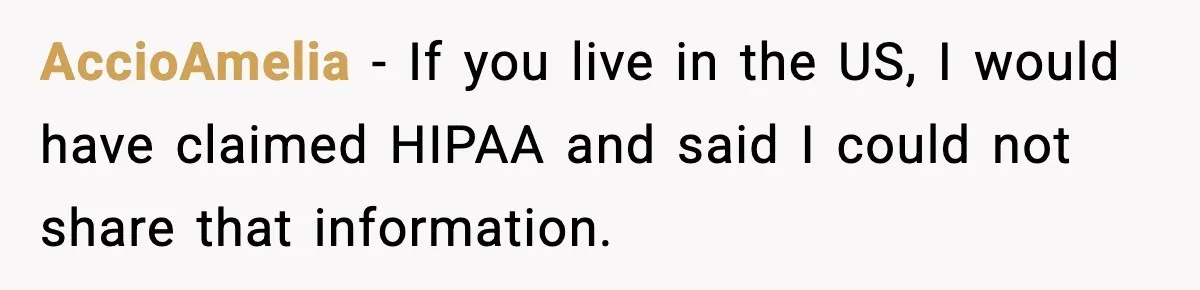
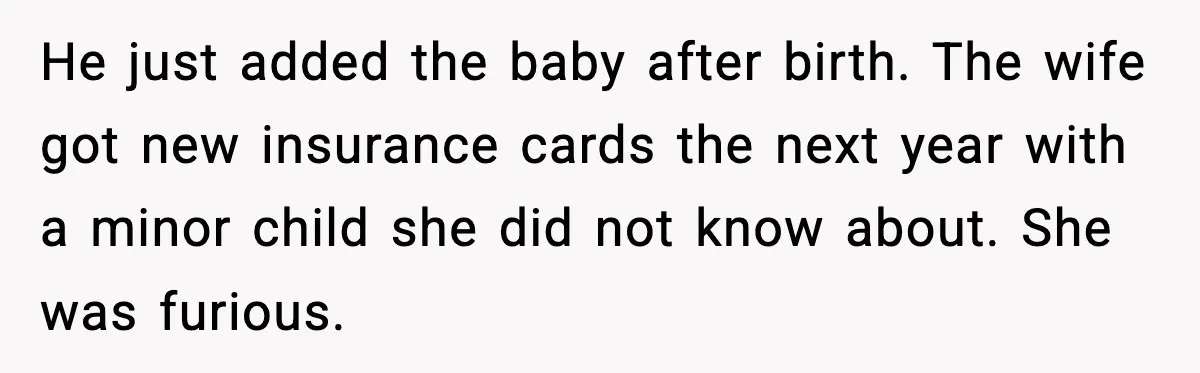
Many readers said OP followed the file and the boss’s orders. They praised her for doing the right thing and saw the fallout as the cheater’s problem, not hers.
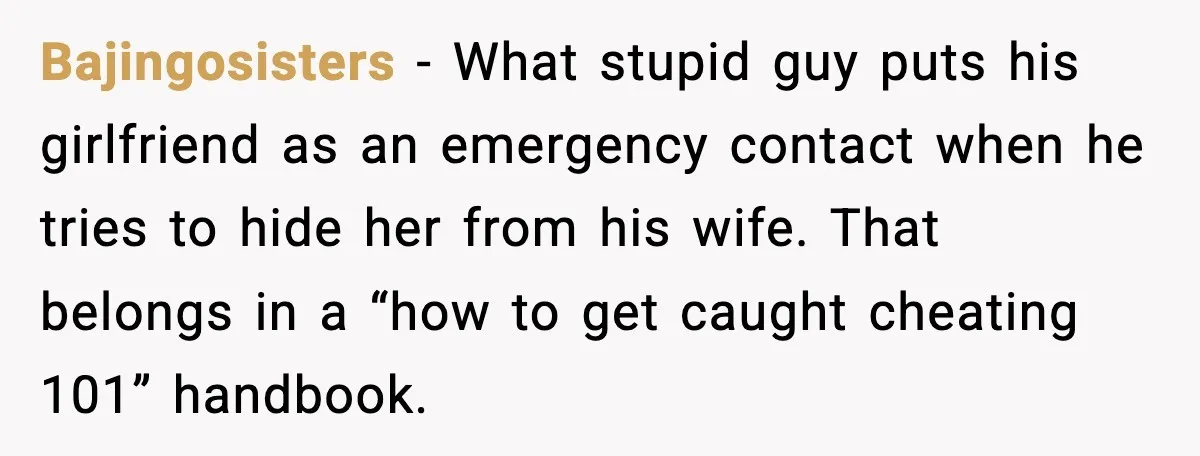
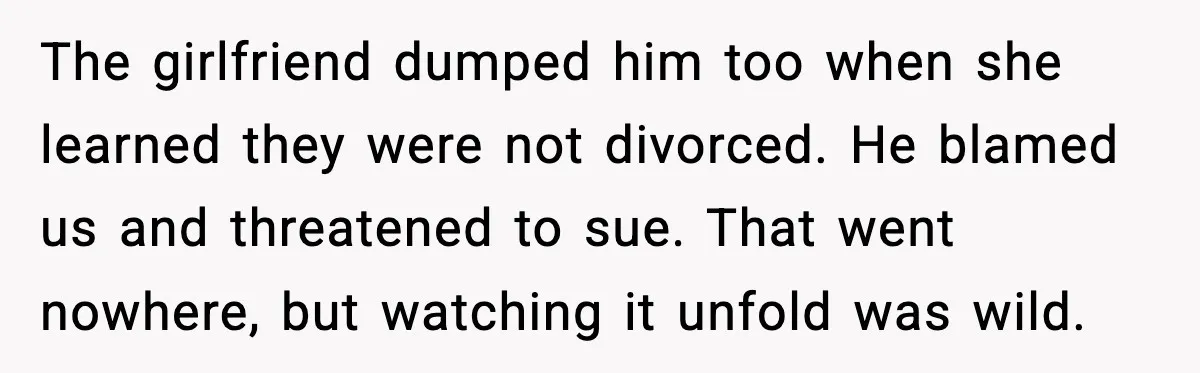
![Cheating Patient Lists Mistress As Emergency Contact And It Backfires Hard [Reddit User] - You were 100 percent right about calling her. I do not know if you should have told the wife who picked them up. Your doctor’s office needed...](https://dailyhighlight.com/wp-content/uploads/2025/11/wp-editor-1763915872050-3.webp)
Commenters had zero patience for the manager. They saw her as the classic boss who loves authority, hates responsibility and treats staff as shields.
Some users dug into the legal side. They pointed out that HIPAA can feel tricky, but OP still sat on solid ground because the wife counted as an authorized person.
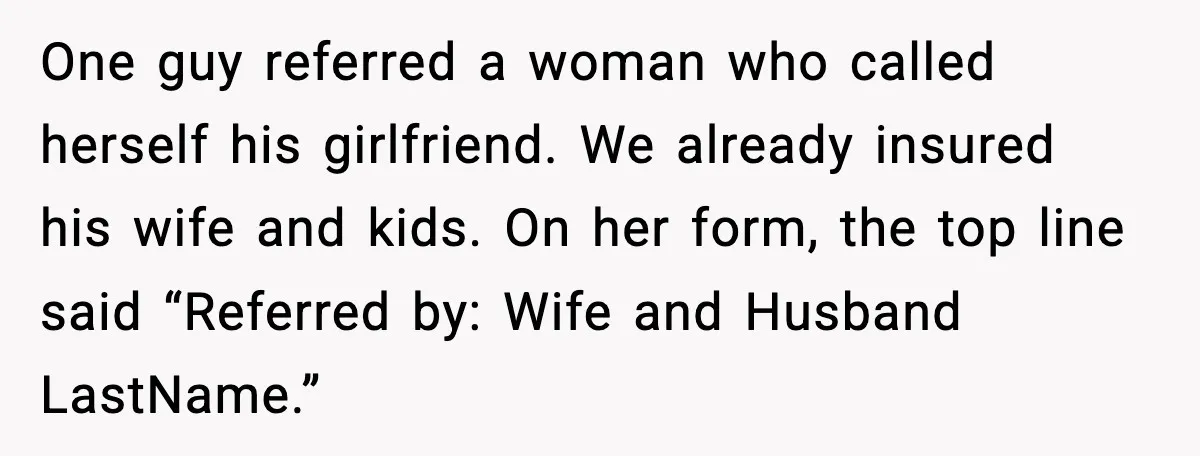
Other Redditors shared their own workplace drama. They talked about insurance, secret girlfriends and how paperwork quietly reveals the truth.

This story wraps together workplace pressure, relationship secrets and the fragile role of front line staff.
The real lesson lives in the choices of the adults around her. Frank wrote his own chaos when he listed his mistress as “girlfriend” in a medical file. Diane cared more about avoiding paperwork than guiding a young worker through an ethical gray area.
The doctor, at least, recognized the context once he heard the full story.
Better systems and better leadership protect both patients and staff. Clear privacy scripts, supportive managers and honest personal lives go a long way.
What would you have done in OP’s place? Would you handle that phone call differently now that you know how fast one name on a form can change everything?