When he opened a bill for his ambulance ride after an anaphylactic reaction, he felt like he had been smacked twice. First the shock of nearly dying.
Then the shock of a large invoice because the hospital-owned ground ambulance that took him in turned out to be out of his insurer’s network. What happened next was equal parts blunt logic and cheeky leverage, and it worked.
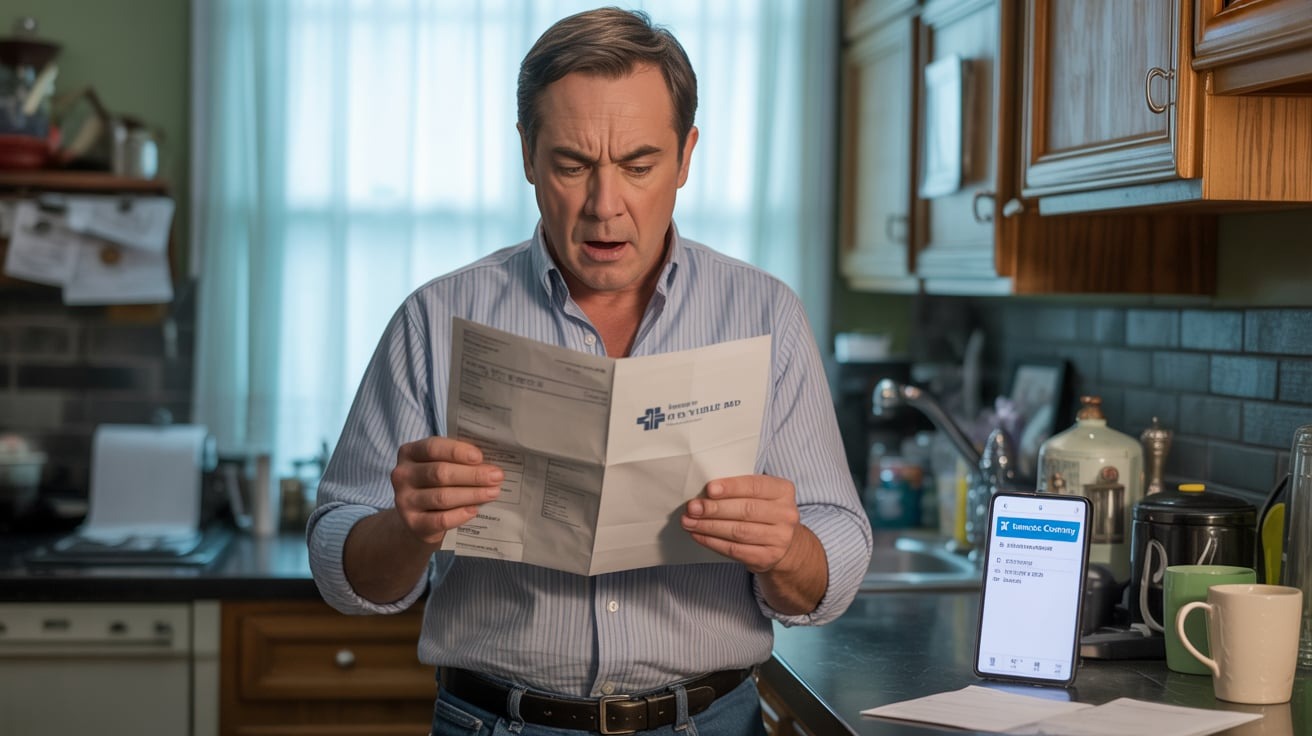
Here’s the original post:
The problem with “in-network” ambulances
After the scare, he called his insurer to ask which ambulance companies were in network within about 150 miles of his rural town. The answer surprised him: almost none.
Ground ambulances in his area were out of network, except for three air ambulance companies. In short, getting to the nearest hospital by driving ambulance could leave you holding a hefty balance, while the only “in-network” option was a helicopter.
That was not a practical or safe expectation for someone who lived three miles from the hospital.
This mismatch is not an isolated quirk. Recent analyses show that out-of-network billing for ambulance rides is common, and the patient financial burden can be significant.
One cross-sectional study found over half of ground ambulance services billed out of network, with average patient financial burdens of several hundred dollars per trip.
Another report noted that nearly 60 percent of ground ambulance rides were out of network in recent years, leaving patients exposed to surprise bills.
Federal protections and their limits
Since 2022, the No Surprises Act has shielded many patients from balance bills for emergency care and for air ambulance services. The law prohibits balance billing in many emergency situations and specifically covers air ambulances from surprise billing.
But ground ambulances are a gray area. While the act tightened protections and created dispute-resolution mechanisms, ground ambulance billing remains a major source of surprise charges for patients in many regions.
In practice, that has left people vulnerable when the nearest or most practical ground ambulance happens to be out of network.
Centers for Medicare & Medicaid Services
His tactic: point out the absurd “in-network” option
When an insurer representative told him the out-of-network bill was by design, to incentivize use of in-network providers, he posed a simple question:
“So your only in-network ambulance is a helicopter, and I live three miles from the hospital. Do you really want me to use that option?”
The rep went quiet, consulted a supervisor, and a week later he received a letter saying his bill was paid in full. It seems the insurer did not relish the optics or logistics of promoting helicopter transport for short, local trips. The nudge worked.
Centers for Medicare & Medicaid Services
Why this matters – practical and ethical angles
From a patient perspective, this is about fairness and safety. People call ambulances in emergencies; they should not have to calculate networks while in distress.
Consumer advocates urge patients to appeal surprise bills and cite federal protections when relevant. In many cases appealing or quoting a plan’s own policy can prompt insurers to cover charges or use the federal dispute process.
One former claims worker advised that emergencies billed out of network should be appealed because many will be reclassified as in-network under the law or plan rules.
Consumer Financial Protection Bureau
Insurers and some policy analysts counter that networks exist to control costs and that having no in-network ground ambulances in a region can reflect market realities, especially in rural areas where ambulance services are municipally run or run by small providers who cannot secure network contracts on insurer terms.
They point out that mandating all ambulances be in network could raise premiums or contract complexity. Yet critics argue market realities cannot justify leaving patients exposed during emergencies, and that federal and state fixes are needed.
What experts suggest
Health policy experts recommend several steps for patients: ask the insurer to explain coverage and in writing; file an appeal citing emergency care protections; request the insurer apply federal No Surprises Act protections if applicable; and if needed, escalate to state insurance regulators or use the federal independent dispute resolution process for unresolved balance bills.
A proactive read of plan documents and quick appeals after a surprising bill often changes outcomes.
Here’s what the community had to contribute:
Redditors were predictably angry and not surprised.
Many shared horror stories of out-of-network labs or anesthesiologists.
Several urged appeals and pointed to the No Surprises Act.
Others expressed broader frustration, calling for fundamental reform to stop profit incentives from jeopardizing emergency care.

His blunt hypothetical – “want me to take a helicopter instead?” – exposed an ugly truth: network rules can produce bizarre, unsafe incentives in emergencies.
He did not invent a legal argument. He simply highlighted a real-world absurdity, and it got his bill wiped.
The fix should not rely on rhetorical helicopters. It should be systemic: clearer rules, better network design in rural areas, and enforcement that emergency care never becomes a surprise financial risk.
Would you have pushed back the same way, or let a scary bill slide?