A hospital room meant for healing turned into a front-row seat to cruelty.
A 23-year-old woman, hospitalized after nearly dying from a severe virus, thought her biggest battle was behind her. Sharing a room with a kind 78-year-old woman, she found comfort in quiet companionship and daily visits from her own father.
But when her dad stepped out one day, something disturbing unfolded.
Her roommate’s usual rotation of loving family members broke. In their place came a son-in-law whose behavior crossed every line imaginable. Instead of comfort, he delivered mockery. Instead of care, he hurled abuse.
The young patient listened in disbelief as the elderly woman, already in pain, endured laughter, curses, and comments about her dying faster so others could collect inheritance money. The cruelty wasn’t subtle. It was constant.
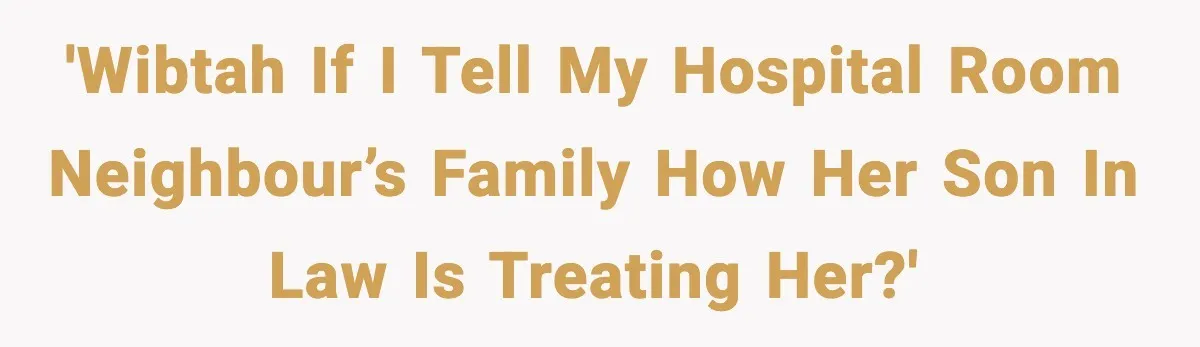
Now, the young woman faces a heavy question. Should she speak up and tell the family what she overheard, or would that make things worse?
It’s the kind of situation no one prepares you for, especially when you’re still trying to recover yourself.
Now, read the full story:
This is one of those stories that makes your stomach drop. You’re already vulnerable in a hospital bed, and suddenly you’re forced to witness emotional abuse happening in real time. The cruelty described here isn’t awkward or misunderstood. It’s deliberate, repeated, and deeply disturbing.
What stands out most is how powerless the elderly woman seems in that moment. She’s in pain. She’s dependent. And the person sitting beside her is exploiting that vulnerability.
The fact that a stranger, barely out of college, feels more protective than a family member says everything. This isn’t drama. This is a safety issue. And that’s where things shift from “Would I be rude?” to “Would I be responsible?”
What this young woman witnessed aligns with recognized forms of elder abuse, specifically emotional and psychological abuse.
According to the World Health Organization, elder abuse includes “acts or omissions that cause harm or distress to an older person,” particularly in relationships where trust is expected. Verbal humiliation, threats, and exploitation related to inheritance all fall squarely into this category.
Hospitals are considered high-risk environments for detecting elder abuse because patients are often isolated, medicated, or physically unable to advocate for themselves. That’s why healthcare staff receive training on recognizing and responding to warning signs.
Dr. Mark Lachs, a geriatrician and co-author of Treating Elder Abuse, explains that emotional abuse is one of the most underreported forms because it leaves no visible marks. Yet, its impact can be just as damaging as physical harm.
In this scenario, several red flags appear at once.
First, the son-in-law openly mocks the patient’s pain. Second, he repeatedly references her death as something desirable. Third, he ties her death to financial gain. Each behavior alone is concerning. Together, they suggest a pattern of hostility and potential exploitation.
Many people in similar situations hesitate to speak up because they fear overstepping. But experts emphasize that bystanders play a crucial role.
The National Center on Elder Abuse advises that if someone suspects abuse in a care setting, the first step should always be notifying medical staff. Nurses and social workers are mandated reporters. That means they are legally required to assess and escalate concerns when abuse is suspected.
Importantly, the responsibility does not fall on the bystander to investigate or confront the abuser. In fact, direct confrontation can sometimes increase risk to the victim later.
By reporting concerns to nurses, several protections activate. Hospital social workers can limit visitor access, document incidents, and coordinate with adult protective services if necessary. This creates a record, which is critical if patterns continue after discharge.
Another common question is whether telling the family is appropriate. Ethically, transparency matters, but experts recommend prioritizing professional channels first. Families are emotionally involved and may react defensively or dismissively, especially if the abuser is related by marriage.
Dr. Laura Mosqueda, director of the National Center on Elder Abuse, notes that abuse often hides behind family dynamics. Outsiders who speak up frequently become the catalyst for intervention.
From a moral standpoint, silence often protects the wrong person.
The young woman asking this question shows empathy and awareness. She’s not seeking drama. She’s seeking safety for someone who may not be able to ask for it herself.
The most responsible action is clear.
Report what you heard to hospital staff immediately. Let trained professionals take it from there. If appropriate, families can be informed through official channels.
Speaking up in situations like this isn’t interference. It’s protection.
Check out how the community responded:
Most commenters urged immediate action through hospital staff.
Others stressed the seriousness of elder abuse and documentation.
Some encouraged notifying family once safety steps are taken.
Situations like this force ordinary people into extraordinary moral moments.
This young woman didn’t ask to witness abuse. She didn’t ask to become involved. But once you hear cruelty this explicit, choosing silence becomes a choice too.
Elder abuse often thrives because it hides in plain sight, dismissed as family conflict or dark humor. But laughing at pain, urging death, and talking about inheritance crosses into something far more dangerous.
The good news is that hospitals are one of the safest places to intervene. Nurses, doctors, and social workers have both the authority and obligation to act.
Speaking up doesn’t make someone a troublemaker. It makes them a safeguard.
So what do you think? If you overheard something this disturbing, would you step in? Or would you struggle with the fear of getting involved?