Expecting a child is an exciting time, filled with anticipation and joy, but it also brings new responsibilities.
For one expectant mother, her excitement is tinged with concern about the health risks her newborn may face.
As flu, RSV, and COVID season approaches, she’s set a clear boundary for her parents, get vaccinated before meeting their grandchild.
However, this request, made with the intention of protecting her baby, has led to a deep divide.

Even well‑intended boundaries can trigger deep family conflict, especially when the emotional stakes are high.
In this case, the OP asked her parents to be vaccinated against COVID‑19, flu, and other respiratory illnesses before visiting her newborn, a reasonable boundary grounded in concern for her child’s health.
Newborns, particularly those under six months old, are too young to be vaccinated for many serious respiratory viruses, yet are among the highest‑risk groups for hospitalization due to COVID‑19 and other infections.
Infants under 6 months have consistently shown higher hospitalization rates than older children, and maternal vaccination offers some passive protection early in life when the baby’s immune system is still developing.
The CDC specifically recommends that everyone around a baby, including parents, siblings, caregivers, and visitors, stay up to date with recommended vaccines such as flu shots each season because infants can’t get these vaccines themselves.
RSV, another common seasonal threat, is the leading cause of infant hospitalization in the U.S., and vaccination of close contacts can help reduce the spread of this virus.
These public health recommendations highlight why the OP’s boundary was medically informed and focused on reducing risk during a particularly vulnerable period.
But boundaries rooted in science don’t always land easily when they collide with personal beliefs.
Many vaccine‑hesitant individuals don’t see their stance as rejection of evidence; rather, they frame their choices around autonomy, risk perception, and individual health priorities.
Sociologist Jennifer Reich, who has studied vaccine hesitancy extensively, explains that some parents prioritize individualized decision‑making and personal management of risk over broad public health recommendations.
This insight helps explain the parents’ reaction, they likely saw the request not as protective but as an encroachment on their personal beliefs and freedoms.
Expert anthropologist Dr. Heidi J. Larson emphasizes that vaccine hesitancy is often less about factual knowledge and more about trust and emotional context.
She notes that understanding the underlying reasons for vaccine resistance, such as fear, identity, or mistrust, can be more effective than simply presenting more data.
This suggests that approaching her parents’ concerns with empathy and curiosity might be more productive than confrontation.
At the same time, the OP’s emotions are valid: she’s contemplating one of the most significant life transitions, and her instinct to protect her newborn reflects parental responsibility.
She can start by reaffirming her boundary while also inviting open conversation.
Rather than positioning vaccination as a test of loyalty, framing it as shared concern for the baby’s well‑being and discussing specific risks and professional guidance could soften defensiveness.
A pediatrician or trusted healthcare provider could help clarify why vaccines for adults and caregivers, not just for the baby, reduce risk.
In family dynamics like this, neither side is purely right or wrong; they’re interpreting health, risk, and love through different lenses.
The OP’s experience shows that protecting a newborn isn’t only biological, it’s emotional and relational.
In the end, setting boundaries based on medical evidence and safety deserves respect, but blending that with empathetic dialogue might help transform hurt into understanding.
Let’s dive into the reactions from Reddit:
These commenters all agree that the OP is in the right. They highlight the dangers of pertussis, RSV, and COVID-19, all of which can be deadly to babies.
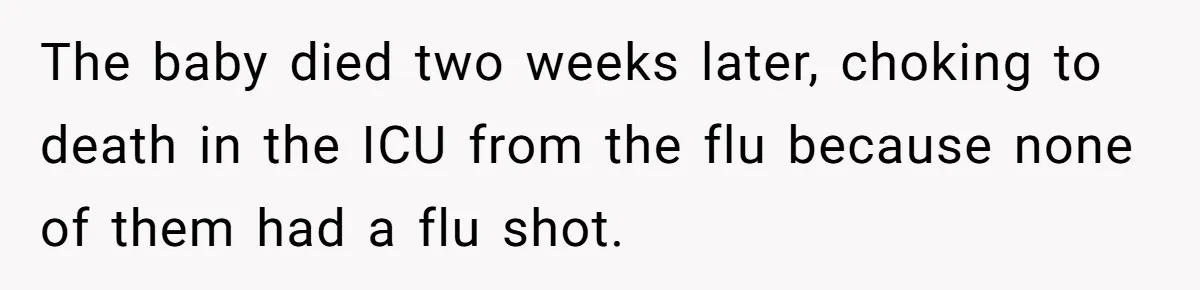
These commenters strongly back the OP’s stance, recalling personal experiences or family stories of loss and illness due to unvaccinated visitors.
hese users note the necessity of firm boundaries, pointing out that if family members truly care, they will prioritize the baby’s well-being by following safety measures.
These commenters are particularly passionate about the dangers of RSV, emphasizing the emotional and physical toll it can take on babies.


The OP’s desire to protect her newborn from potential illness is entirely understandable, but the boundary she set has clearly caused tension with her parents.
It’s clear her intentions are rooted in love and concern for her child’s health, but with parents who refuse to cooperate, was she too firm in her stance?
How would you navigate a situation where your protective instincts clash with family expectations? Share your thoughts below!